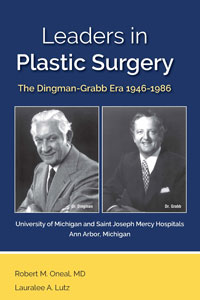
Leaders in Plastic Surgery
Skip other details (including permanent urls, DOI, citation information): This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 3.0 License. Please contact [email protected] to use this work in a way not covered by the license.
For more information, read Michigan Publishing's access and usage policy.
Introduction of Craniofacial Surgery to Michigan
Dr. Haskell Newman related in detail the sequence of events that brought craniofacial surgery to Michigan and its subsequent developments:
In 1967, Dr. Paul Tessier presented the first successful case in which a facial advancement was performed to treat a patient with Crouzon Syndrome. A publication described the technique.[143] A Le Fort III osteotomy advancement was designed to include a major portion of the orbits with the upper jaw. This technique of dissecting tissue from the facial bones with simultaneous intracranial exposure and circumferential mobilization of the orbits enabled repositioning of the eyes and the skull. Tessier’s techniques are based on the principle that skull and facial bones must be repositioned or reconstructed before soft tissue can be repaired. In the early 1970s, surgeons from the United States visited Tessier to learn the new operative techniques. Among his early students was Reed Dingman, Chairman of the Section of Plastic Surgery at the University of Michigan.[144]
Dr. Glass (1970–71) also recalled that “as soon as Paul Tessier (from France) told the world about his work, ROD had the guts, interest, and stamina to embrace this new discipline called craniofacial surgery and started doing cases.”[145] Dr. Newman continued, “In 1970, Dr Dingman initiated craniofacial surgery at the university when he accomplished the surgical correction of a patient with Crouzon craniofacial deformity assisted by a university neurosurgeon and Dr. John Converse, the chairman of plastic surgery, New York University”[146] (Photo 58). This event was remembered by Dr. Hudak who recounted, “One of our most interesting visiting professors was John Converse. We had the opportunity to see him and Dr. Dingman operate on a child with Crouzon Syndrome. That was a unique experience for all who witnessed the operation. It took place in the year 1969–70, which was my second year as resident.”[147] Dr. Wexler recollected a subsequent case that took place in 1972.[148]
Dr. Newman recalled,
In the fall of that year, I was an assistant professor in the Department of Otolaryngology and I applied for a residency position in plastic surgery. The interview with Dr. Dingman centered on a joint interest in the developing specialty of craniofacial surgery. After completing the residency in plastic surgery, encouraged by Drs. Dingman and Grabb, I completed a fellowship of craniofacial surgery with Dr. Ian Munro at the University of Toronto, and in 1978, I was recruited by Dr. Grabb to establish a multidisciplinary team to provide consistency and safety with the most advanced treatment for patients suffering from craniofacial anomalies.
The plastic surgery faculty with interest and training in the correction of craniofacial anomalies was expanded in 1981 with the addition of Dr. Lou Argenta following his fellowship training with Dr. Tessier in Paris [Photo 59]. In 1982, Dr. Newman confined his practice to SJMH and Dr. Argenta directed the craniofacial program at the University of Michigan Hospital systems until his departure in 1988. Adult craniofacial and maxillofacial surgery and specialty training were expanded in practices at the university hospital and SJMH. Neurosurgical participation in the craniofacial program was enhanced when, in 1983, Dr. Joan Venes was recruited to establish and head a division of pediatric neurosurgery. Through the combined interest and efforts of Dr. Venes and the plastic surgery faculty, craniofacial surgical focus expanded to include early interventional correction of craniofacial deformities in infants and young children.[149]




