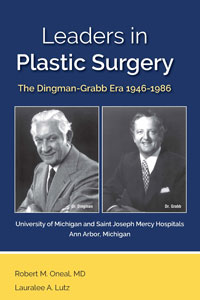
Leaders in Plastic Surgery
Skip other details (including permanent urls, DOI, citation information): This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 3.0 License. Please contact [email protected] to use this work in a way not covered by the license.
For more information, read Michigan Publishing's access and usage policy.
Early Work of Dr. Dingman and Dr. Grabb
Prior to his plastic surgery training with Dr. Ferris Smith that was completed in 1946, Dr. Dingman’s curriculum vitae (CV) indicated his clinical activity was mostly limited to oral surgery conditions and concerns. One exception was an article in 1939 in the Archives of Otolaryngology about periocular sinuses. The other published subjects include management of facial fractures, osteomyelitis and tumors of the jaws, abnormalities of the temporomandibular joint (TMJ), and orthognathic surgery. However, beginning in 1948 and up until Dr. Grabb joined him in 1961, Dr. Dingman’s emphasis shifted to subjects more of an interest to plastic surgeons. In 1948, he published an article on surgical correction of developmental deformities of the mandible in the second volume of the Plastic and Reconstructive Surgery (PRS) journal.[1] This was followed by articles on such varied subjects as cleft lip,[2] iliac bone grafts,[3] malunion of facial fractures,[4] Z-plasty,[5] radiated costal cartilage,[6] ostectomy of the mandible in cleft lip and cleft palate patients,[7] and rhinoplasty caused by defects of the septum.[8] In 1961, when Dr. Grabb was a resident and coauthor, two articles were published, one on lymphangioma of the tongue[9] and the other on human rib cartilage grafts preserved by irradiation.
The latter article turned out to be an important contribution to facial reconstruction. The following is quoted from the introduction to the 1961 PRS article by Dingman and Grabb[10]: “Preserved costal cartilage homografts have proven to be of value in restoring contour defects of the supporting structures of the face. The cartilage can be sterilized and preserved indefinitely. It can be easily sculptured at the operating table and after implantation it is well tolerated by the body tissue.” Dr. Dingman quoted an earlier article from 1956,[11] where he and two others reported the use of irradiation to sterilize canine costal cartilage, and it was subsequently determined that sterilization of human costal cartilage could be accomplished by rapid (fifteen hours) cobalt 69 gamma irradiation using 3,000,000 rep. This was carried out in the Ford Nuclear Reactor in the Phoenix Memorial Laboratory at the UM.
The cartilage was obtained at autopsy, ideally from young adults, and was refrigerated and stored until it could be prepared by a resident assigned to this project. The cartilage was stripped of soft tissues and the perichondrium was preserved. It was then cut into lengths to fit into a glass canning jar filled with saline and tightly sealed. After sterilization by the irradiation, the cartilage is ready for use the next day or can be stored indefinitely. The article reported that twenty-eight of thirty human patients receiving these grafts for chin augmentation, orbital floor defects, and dorsum of the nose showed no clinical evidence of absorption in seven months to 3½ years postoperatively. (The two that absorbed were used for external ear reconstruction where autologous cartilage is essential for success.) This knowledge of the successful utilization of homograft cartilage was essential in our reconstructive efforts as there were few other materials available or more dependable for many years after this report. We all kept a few of these jars containing the irradiated cartilage close at hand in the operating room (OR) suite for many years. Illustrative of Dr. Dingman’s intellectual generosity is the statement in the summary in the 1961 article that the arrangements for the resources of the Phoenix lab at the UM would be available for others interested in adopting this technique.[12] Dr. Wexler sent his recollection about the cartilage collection (which has undergone some minor editing):
Twice a month we went to the morgue, opened chests, cutting the out cartilaginous part of the ribs [cutting ribs in to 4 cm lengths], then put them into saline-filled transparent glass jars. They were taken to the atomic reactor on North Campus, irradiated with 3 million rads and the jars became brown. We kept the jars on the shelves ready to be used as filling material—similar to the silicones today. This was excellent, curvable, infection resistant material. One evening, in the winter, I took a bar [of cartilage] to be used at Jackson prison. I left it in my car. Next morning I found a block of ice in the car surrounded with broken glass. What happened to the cartilage? I do not recall exactly. Why might it have been taken and what to be used for?[13]
Paul Izenberg recalled six years later that the cadaver cartilage was still being collected: “I remember being called into the section office by Lauralee and being told ‘it’s time’ knowing that the task of harvesting cartilage for processing was upon us. So a couple of us (usually junior residents) hiked over the cadaver lab to process the specimens.”[14] Paul suggests that this denatured homograft material was, in a way, a forerunner of acellular dermal matrix, now one of the most often used homografts in plastic surgery.[15]
In further review of Dr. Dingman’s CV, it was noted that starting around the time in 1952 when he turned down the chairmanship of oral surgery at the dental school and aligned himself with the surgery department at the medical school, he had published a series of articles during the subsequent ten years, either collaborating with someone from another specialty in the medical center or on a subject only peripherally related to plastic surgery but published in one of the other specialty journals. Examples include an article about Z-plasty to the urethral meatus, published with Dr. Reed Nesbit who was chairman of the urology department; an article about cheilitis glandularis with reconstruction of the upper lip, with Dr. Arthur “Whitey” Curtis who was head of the dermatology department; and an article about semi-open burn management, with Dr. Irving Feller, a member of the general surgery section and on his way to becoming a burn specialist who was responsible for setting up the Burn Unit at UM. Examples of the second category include an article about necrobiosis lipoidica diabeticorum published in AMA Archives of Dermatology and Syphilology 1951,[16] one regarding a malunion of the zygoma in the Transactions of the American Academy of Ophthalmology,[17] and another about a burn scar contracture of the neck in the Surgery Clinics of North America. While noting the subjects and coauthors of these various publications, it occurred to me that perhaps during those ten or so years, Dr. Dingman was making a concerted effort to reach out and show the applicability of basic plastic surgery principles in the management of a wide variety of medical and surgical problems. He was also trying to heighten awareness of the value of having plastic surgery as a readily available consulting service within a major medical center. Perhaps just as important were his efforts toward building rapport among the medical staff to gain support for the ultimate formation of a plastic surgery section in the medical center within the Department of Surgery.
Subsequently, the range of continuing and varied interests, as shown in his list of publications, continued to expand rapidly. Some of the subjects included management of tumors, wound healing, and Z-plasty. A particular interest involved facial injuries associated with auto accidents. This led to a series of articles from 1960 to 1968, published together with Dr. Grabb and Dr. Donald Huelke, a professor in the anatomy department and a research scientist at the UM Transportation Research Institute. The subjects included facial injuries due to windshield impacts injuries and deaths from windshield and instrument panel impacts. One of the most significant findings, published in 1968, concerned the decrease in frequency and severity of facial lacerations after introduction of the new automobile windshield design.[18] This new design almost single-handedly eradicated the frequent and extensive facial lacerations (one to three patients a week seen in our emergency rooms) that resulted from the vehicle’s occupant’s head penetrating the older design windshields in front-end collisions (no seat belts in those days).
Along the way, new instruments were introduced. The first was a bone and cartilage grasping forceps in 1954[19] that became widely used. The next was a newly designed plastic surgery dressing cart for use in hospitals and modifiable for use in other specialties. The details of the design were published in 1957 with coauthors Dr. Paul Natvig, who was still a plastic surgery resident, and Jim Winkler, who was then a resident in general surgery at Saint Joseph Mercy Hospital (SJMH).[20] In 1965, with Dr. Grabb as coauthor, Dr. Dingman introduced the now universally used Dingman mouth gag for cleft palate repair in 1962 (discussed, with photo, on pp. 99–100).[21] He also developed the double-ended Dingman periosteal elevator, the Dingman ear abrader (described under the discussion of otoplasty, p. 107), and the transaxillary augmentation mammoplasty dissector (described in the section on augmentation mammoplasty, p. 90).
It is difficult to summarize the enormous clinical output of the next several years. Dr. Dingman’s interest in innovations and clinical problems encompassed a wide range of subjects in addition to those already mentioned: facial reconstruction; face, brow, and eyelid surgery; rhinoplasty; otoplasty; scalp and lip reconstruction; cleft lip repair; other developmental abnormalities; chest wall reconstruction; treatment of multiple types of benign and malignant lesions; and TMJ surgery.
In 1964, there was an important article on TMJ reconstruction with metatarsal grafts by Dr. Dingman with Dr. Grabb as coauthor.[22] The article reported and described the technique Dr. Dingman developed for treating a twenty-nine-year-old female to correct the deformity resulting from a previous operation, ten years earlier, when a surgeon had removed her bilateral mandibular condyles as a radical method to treat intractable TMJ symptoms. On presentation, she had a severe open bite with only her molar teeth in occlusion. Restoration of the condyles was accomplished by using the heads of the bilateral fifth metatarsal bones as fresh autogenous grafts. The patient was followed for seventeen months, and x-rays showed transplanted bone to be intact, and normal occlusion and mandibular function restored, with markedly improved speech. She had no complaints with her feet and was wearing only a slightly narrower shoe than before. The authors drew the conclusion that half-joint transplants do not undergo the destructive changes of bone and cartilage that occur in whole joint transplants. This was a very significant finding. Interestingly, several months later, the patient had an irradiated costal cartilage graft to correct her retruding chin deformity. A 1975 article (referenced and discussed in p. 114) reported an additional eight more cases using metatarsal grafts in a variety of deformities of the TMJ, all with satisfactory results.
There were several articles published and many coauthored with Dr. Grabb on various aspects of both acute traumatic and secondary deformities of facial bones. Of course, the highpoint of the published work on that subject was Drs. Dingman and Natvig’s book titled Surgery of Facial Fractures, published in 1964 (Photo 52). It became the “bible” for the treatment of facial fractures (referenced and discussed in p. 112). Dr. Dingman always encouraged and invited both his colleagues and residents to join him in these many projects that resulted in publications. That continued well beyond his retirement as section head.
In those early years, in addition to Dr. Grabb and myself, there were faculty members from many disciplines as coauthors with Dr. Dingman. These included Dr. Harlan Bloomer, director of the speech clinic; Dr. Donald Huelke; Gerald Hodge, head of medical illustration; and Dr. Robert Ponitz, DDS, an orthodontist in private practice who worked closely with all of us in our orthognathic cases as well as consulting in the SJMH Cleft Palate Clinic. The list also includes Krystyna Pasyk, PhD, who was an active participant for many years in the Sargent laboratory, and Dr. Gary Sandall, a pediatric ophthalmologist. Examples from the resident/fellow group of coauthors through these years and beyond include James Winkler; Jim Bennett; Bob Knode; Ralph Seaton; John Markley, who was a student at the time; Eric Constant; Don Davis; Grant Fairbanks; Ron Wexler; Joe Agris; Bob Wilensky; Isaac Peled; Paul Izenberg; Paul Dempsey; Paul Natvig; Bob Gilman; and Malcolm Marks.
When Dr. Grabb completed his residency, he joined Dr. Dingman in practice at SJMH. From the very beginning, he brought innumerable ideas and much energy to the academic side of the residency training program. One example is the clinical study of the anatomy of the mandibular ramus of the seventh nerve published together with Dr. Dingman in 1962.[23] One hundred human facial halves were dissected with cooperation from Dr. Russell Woodburn, head of the Department of Anatomy. Dr. Woodburn was a wonderful and inspiring teacher and friend to all surgeons who were interested in the details of anatomy. This study, carried out on embalmed cadavers, defined that the position of the mandibular ramus, anterior to the facial artery, was always above the lower border of the mandible. At the posterior, the branch or branches were often below the mandibular border, and this was a warning to the surgeon approaching this area to undertake an open reduction of the mandible. This study was well received and referred to often in the OR.
Breaking new ground, five years later, Dr. Grabb published an important study that described and clarified the characteristics of the first and second branchial arch syndrome.[24] This syndrome was defined as a constellation of abnormalities resulting in a spectrum of facial malformations that blend with one another and have no bold or clear lines of delineation. The paper was based on a study of 102 patients who were identified by birth records at SJMH and who agreed to return for clinical evaluation. This was a pioneering study and very well regarded at the time. It was an important step leading to a new and clearer idea of a “sequence,” which defines the spectrum of anomalies found within types of congenital facial deformities.
As mentioned in detail under his tenure as section head and so beautifully stated in Dr. Dingman’s eulogy, Bill Grabb was a prolific researcher, writer, and teacher in addition to being an inspirational and highly respected leader.



