Prevalence and Risk Factors of Postpartum Depression in Middle Eastern/Arab Women
Skip other details (including permanent urls, DOI, citation information)
: This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 3.0 License. Please contact mpub-help@umich.edu to use this work in a way not covered by the license.
For more information, read Michigan Publishing's access and usage policy.
Abstract
Minimal research is available on postpartum depression (PPD) in women from the Middle East/Arab countries. A literature search revealed only 21 empirical studies conducted in the Arab world in the last 20 years. This paper attempts to analyze the existing data for prevalence and risk factors associated with PPD in the target population. The results of review are discussed with implications for prevention and treatment.
Keywords: Postpartum Depression, risk factors, cultural considerations, Middle Eastern, Arab women.
Postpartum Depression (PPD) affects women around the world and it is estimated that its prevalence runs at about 10-15% (Fuggle, Glover, Khan & Haydon, 2002). Some studies show that PPD may affect up to 30% of all women after delivery (Evins, Theofrastous & Galvin, 2000; WHO, 2003), and has a significant impact on the mother and long-term consequences on the cognitive and emotional development of children (Tammentie, Tarka, Astedt-Kurki & Paavilainen, 2002). It is generally also agreed that while this illness can turn into major depression and carries substantial risk of morbidity and death, it is an underdiagnosed and underrated illness. Mathers & Loncar (2006) project that by the year 2030, depression will be one of the top three leading causes of death in the world; yet PPD is one of the least addressed types of depression today. Additionally, for women who have experienced PPD, up to 50% will face a reoccurrence during subsequent pregnancies (Nonacs and Cohen, 2000). PPD typically occurs within the first three months after childbirth, lasts a minimum of two weeks, and can cause clinically significant impairment in daily functioning (Reck et al., 2008). According to the World Health Organization (2003), PPD symptoms include feelings of anxiety, hopelessness, decreased appetite, inability to concentrate, decreased interest in the baby or life in general, and altered sleep patterns. However, clear guidelines for diagnosing PPD is still lacking in the DSM (Segre & Davis, 2013).
The Diagnostic and Statistical Manual (DSM), which is considered “the bible” of diagnostic and classification of mental disorders, did not recognize PPD until its fourth edition published in 1994. Major Depressive Disorder (MDD) in the DSM-IV-TR (APA, 1994) included a list of specifiers to describe mood episodes one of which was “postpartum onset occurring within four weeks of delivering a baby.” The DSM-5 also does not recognize PPD as a separate disorder; rather, patients must meet the criteria for MDD and the criteria for peripartum-onset specifier referring to “the most recent episode occurring during pregnancy as well as in the four weeks following delivery.” (See Table 1 for the DSM-5 criteria for MDD.) The DSM-5 now also acknowledges coexisting symptoms of anxiety and panic (Stone, 2013). As the DSM is based primarily on data from Western population, the diagnosis of psychiatric disorders for people of nonwestern backgrounds becomes challenging (Haque, 2010; Roysircar, 2005). This is particularly true for PPD, as it is not fully understood and addressed in the DSM and is manifested differently in different parts of the world. Timely diagnosis and treatment of PPD is essential not only for women’s own mental health but also because such symptoms can lead to poor maternal-infant bonding and disrupt the infant’s own emotional and cognitive development if left untreated (Grace, Evinden, & Stewart, 2003). Detrimental effects of misdiagnosed and untreated PPD include poor relationships and interpersonal interactions, substance abuse, infanticide, and suicide (Wisner, Chambers, & Sit, 2006), poor quality of life (Beck, 1993) and recurrent depressive episodes in future pregnancies (Gabbe et al., 2007).
Table 1. A Synopsis of the DSM-5 Criteria for Manic Depressive Episode with Postpartum Onset*
The DSM-5 criteria for a major depressive episode are as follows:
- Five or more out of 9 symptoms (including at least one of depressed mood and loss of interest or pleasure) in the same 2-week period. Each of these symptoms represents a change from previous functioning, and needs to be present nearly every day:
- Depressed mood (subjective or observed); can be irritable mood in children and adolescents, most of the day;
- Loss of interest or pleasure, most of the day;
- Change in weight or appetite. Weight: 5 percent change over 1 month;
- Insomnia or hypersomnia;
- Psychomotor retardation or agitation (observed);
- Loss of energy or fatigue;
- Worthlessness or guilt;
- Impaired concentration or indecisiveness; or
- Recurrent thoughts of death or suicidal ideation or attempt.
- Symptoms cause significant distress or impairment.
- Episode is not attributable to a substance or medical condition.
- Episode is not better explained by a psychotic disorder.
- There has never been a manic or hypomanic episode. Exclusion e) does not apply if a (hypo)manic episode was substance-induced or attributable to a medical condition.
- “Postpartum Onset Specifier” if the current onset of symptoms is within four weeks following childbirth.
Note: This list is presented to increase awareness of the DSM Guidelines on criteria for diagnosing depression during postpartum period and may not include all symptoms of PPD. This should not be the only tool to diagnose PPD. Additionally, while PPD is the most common affective disorder, the most severe disorders that occurs during postpartum period is postpartum psychosis (1-2%) when the mother experience psychotic thoughts. Postpartum Anxiety Disorders are more common and if left untreated may develop into PPD.
*American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edition, Washington DC: APA 2013.
Because of the keen interest in the emotional wellbeing and mental health of pregnant and postpartum women and accompanying psychiatric diagnostic developments, there is significant amount of research on this topic but very little is written on women from the Middle East and Arab countries (Klanin & Arthur, 2009; O’Mahoney & Donnelly, 2010). It is therefore essential to know the nature and extent of this problem as a lack of such knowledge has serious implications for diagnosis and treatment. Also, as research supports a decrease in depressive symptomatology when treatment is provided, it is essential that all societies recognize and build awareness of the risk factors associated with this illness (Bowen, Bowen, Butt, Rahman, & Muhajarine, 2012). This paper aims to examine the existing literature on the prevalence and risk factors in PPD and discuss implications for prevention and treatment.
Methods
A literature review was undertaken by using various electronic research databases including Access Medicine, Psych Info, PubMed, Science Direct, ProQuest Dissertation and Theses, Medline plus and EBSCOHost. Studies qualified for this review if they met the following requirements: (a) examined prevalence and/or risk factors for PPD, (b) utilized a sample of Middle-Eastern/Arab women using quantitative or qualitative methodologies, and (c) were published in English in the last twenty years (1994-2014). Nineteen studies from Middle-Eastern countries were identified, one each from Tunisia and Morocco, and one on Arab women living in Australia. Overall, a total of 22 studies were examined, summarized, synthesized, and included as part of the literature review.
Results
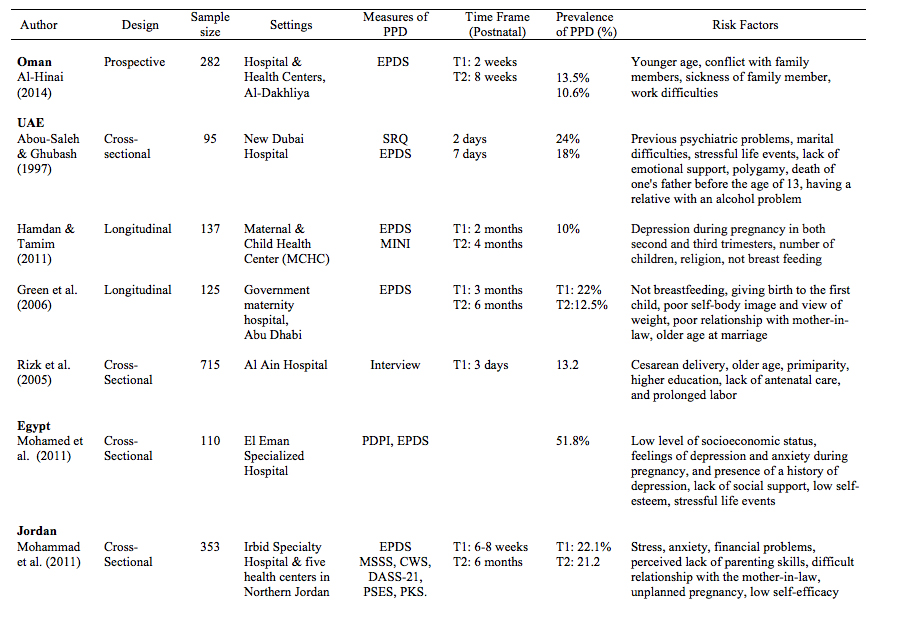
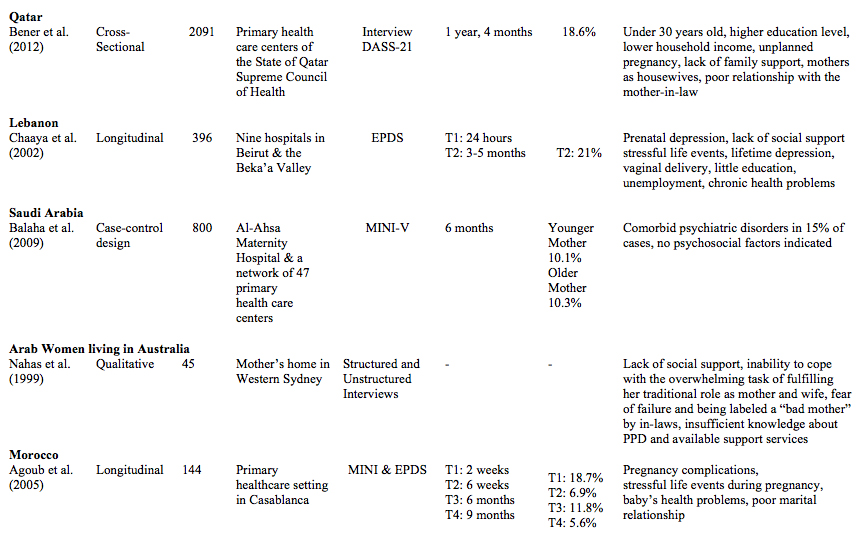
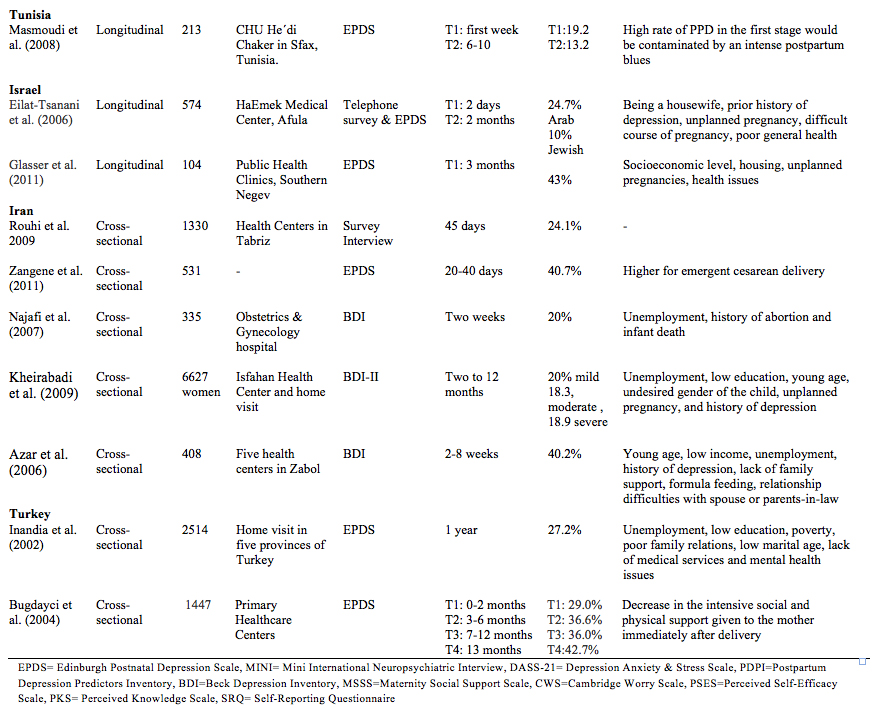
The review resulted in 22 studies on PPD conducted in 12 countries: Oman (n=1), Iran (n=5), United Arab Emirates (n=4), Egypt (n=1) Jordan (n=1), Lebanon (n=1), Saudi Arabia (n=1), Morocco (n=1), Tunisia (n=1), Qatar (n=1), Israel (n=2), Australia (n=1), and Turkey (n=2). Twenty-one studies utilized a quantitative approach while one study used a qualitative method. The majority of studies collected cross-sectional data (n = 13) and used a convenience or purposive sampling with sample sizes ranging from 45 to 6627. Most participants were recruited from hospitals (n=9) followed by primary healthcare clinics and home visits. As shown in Table 2, the Edinburgh Postnatal Depression Scale (EPDS) was the most frequently used instrument (n =14), followed by the Mini International Neuropsychiatric Inventory (n=3), Beck Depression Inventory ( n=3), qualitative interviews (n=3), Depression Anxiety & Stress Scale (n=2), the Postpartum Depression Predictors Inventory (n=1), Maternity Social Support Scale (n=1), Cambridge Worry Scale (n=1), Perceived Self-Efficacy Scale (n=1), and Self-Reporting Questionnaire (n=1).
Prevalence
Based on the review, the prevalence rate of PPD among Middle-Eastern/Arabic women shows a variation ranging from 10%-51.8% within the first few months of delivery. Such variation is also evident in studies conducted within the same country. For example, prevalence rates of PPD in the UAE vary from 10% to 22%. Studies indicate that the range of prevalence rates of PPD in Middle Eastern/Arab countries is greater than the ranges reported in other countries such as the United States (12%), Sweden (13%), Australia (15%), Canada (8%), and Norway (10%), (Segre, O’Hara, Arndt, & Stuart, 2007; Alfonso, De, Horowitz, & Mayberry, 2000; Lanes, Kuk, & Tamim, 2011; Glavin, Smith, Sørum, 2009). These statistics are consistent with a cohort study done by Affonso and colleagues (2000), where the prevalence of PPD and anxiety in women from Asian countries were higher compared to Western countries.
As illustrated in Table 2, studies vary regarding the increase or decrease of PPD during the first year post-partum. Some results show fluctuations during various points (e.g. Agoub, Moussaoui, & Battas, 2005) while a majority showed that the prevalence decreased overtime. In Turkey, Bugdayci, Sasmaz, Tezcan, Kurt, and Öner (2004) showed that prevalence rates increased with time elapsed since delivery.
Risk factors
Studies indicated numerous risk factors that can be categorized into five major groups: physical/biological, psychological, obstetric/pediatric, socio-demographic, and cultural factors.
Physical/Biological Factors
A relationship between physical/biological factors and PPD is reported in 9 studies. Depressive mothers reported a history of psychiatric illness during pregnancy (Abou-Saleh & Ghubash, 1997; Chaaya et al., 2002; Eilat-Tsanani et al., 2006; Hamdan & Tamim, 2011; Inandia et al., 2002; Kheirabadi et al., 2009; Mohamed et al., 2011). Kheirabadi et al. (2009) reported a 35.8% prevalence rate of severe depression (based on BDI score) in women with a previous history of depression. This is consistent with a review of the literature conducted by Alici-Evcimen and Sudak (2003) in the United States. In addition, a history of chronic health problems and a lack of antenatal care are reported (Chaaya et al., 2002; Eilat-Tsanani et al., 2006; Glasser et al. 2011; Rizk et al., 2005). In a study on PPD, Jordanian women also indicated that PPD had a negative physical effect on them (Khalaf, Abu-Moghli, Mahadeen, Callister, & Al-Hadidi, 2007) and presented somatic symptoms including backache, headache, and fatigue as major complaints (Rouhi, Usefi, & Mohamad Alizade, 2009). Eilat-Tsanani and colleagues (2006) showed that women diagnosed with PPD consulted with pediatricians and family physicians about a specific problem more often than those without a PPD diagnosis.
Psychological factors
Psychological risk factors for PPD are extensively studied and several risk factors have been identified. Stressful life events (Abou-Saleh & Ghubash, 1997; Mohamed, et al., 2011; Agoub et al., 2005; Chaaya et al., 2002), marital difficulties (Abou-Saleh & Ghubash, 1997; Agoub et al., 2005), lack of social/emotional support (Abou-Saleh & Ghubash, 1997; Mohamed, et al., 2011; Alkar & Gencoz, 2005; Bugdayci et al., 2004; Nahas et al., 1999; Bener et al., 2012; Chaaya et al., 2002; Azar et al., 2006) and conflict with family members (Al-Hinai, 2014) have been reported.
In one study in the UAE, Green and colleagues (2006) found that body image and weight concerns also seemed to be stressful for postpartum women. Dissatisfaction with their body shape and weight increased the likelihood of more severe depression. A round body was traditionally viewed as beautiful in the region; however, with the influx of Western media, younger women’s views toward desirable body shapes have changed. Although the perception of a thin body as beautiful previously was prevalent in only Western cultures, it is now spreading among Middle Eastern/Arab women.
Low self-esteem, low self-efficacy, and perceived lack of parenting knowledge are among other risk factors identified in these studies (Mohamed et al., 2011; Mohammad et al., 2011). Overall, these studies describe women with PPD as experiencing a range of stressful life events, such as relationship, financial, and maternal stressors while receiving low social/emotional support. Danaci and colleagues (2002) hypothesized that increased PPD may be related to the fact that “mothers receive a great deal of interest and support immediately following the birth but that this drops off over time” contributing to the possibility of higher levels of depression (as cited in Green, Broome, & Mirabella, 2006).
The study of Arab women in the UAE by Ghubash and Eapen (2009) revealed that the majority of women who took part in the study did not recognize postnatal depression as a psychological issue but considered the problem a result of "evil eye" or "Jinn". In another study by Rizk, Nasser, Thomas, and Ezimokhai (2005), 13.2% of mothers in the UAE described their postpartum depression as negative feelings of fear, anger, sorrow, regret, guilt, jealousy, a sense of failure, and disappointment. Interestingly, women who gave birth by cesarean section as opposed to natural delivery reported depressive feelings more often. For women in the West, suicide and suicidal ideation are significant factors associated with PPD diagnosis (Doucet & Letourneau, 2009) but no such findings are currently available for women from Middle East/Arab region.
Obstetric/Pediatric factors
Prolonged labor (Rizk et al., 2005), unplanned pregnancies (Mohammad et al., 2011; Bener et al., 2012; Eilat-Tsanani et al., 2006; Glasser et al. 2011; Kheirabadi et al., 2009), pregnancy complications (Agoub et al., 2005; Eilat-Tsanani et al., 2006), baby’s health problems (Agoub et al., 2005), not breastfeeding (Green et al., 2006; Hamdan & Tamim, 2011), and a history of abortion and infant death (Najafi et al., 2007) are among the obstetric/pediatric factors identified in these studies. Unplanned pregnancy is the most frequently reported obstetric risk factor for PPD. Kheirabadi and colleagues (2009) argued that while an unplanned pregnancy does not necessarily indicate an unaccepted one, women still have to cope with the long-term ramifications such as financial demands that are likely to occur. In this study, undesired gender of the child was also identified as a risk factor (Kheirabadi et al., 2009). The studies give inconsistent findings regarding an association between the mode of delivery and the development of PPD. Among women in Lebanon, vaginal delivery was associated with a higher rate of PPD whereas in the UAE, women who delivered by cesarean section expressed more negative feelings after delivery. A study in Iran showed no significant relationship between these two variables (Sharifi, Sooky, Tagharrobi, & Akbari, 2007). Zangene and colleagues (2011) reported only emergent cesarean as associated with PPD.
Physical complications during delivery or difficulty breastfeeding were also associated with PPD. These factors may symbolize “failure” in the achievement of normative motherhood (Yount & Smith, 2012). In Islam, women are encouraged to breastfeed for two years and various passages in the Qur’an and hadith state the importance of this relationship. Green and colleagues (2006) emphasize not meeting these religious and societal expectations could be stressful and thus increase the likelihood of women experiencing depression.
Studies also identified giving birth to the first child as a risk factor for PPD as some new mothers entering new emotional and physical territory may find it difficult to prepare for the depth of change they will experience (Green et al., 2006). This could equate to a time of higher depression as they struggle to adapt to motherhood. It is also found that multiple deliveries diminish the vulnerability to PPD, due to nonspecific decreases in stress associated with the pregnancy and delivery (Kheirabadi et al., 2009).
Socio-Demographic Factors
The number of children (Hamdan & Tamim, 2011), religiosity (Hamdan & Tamim, 2011), and marriage at an older age (Green et al., 2006) were also identified as risk factors by several studies. In addition, women with a low level of socioeconomic status were found to be at greater risk (Bener et al., 2012; Glasser et al., 2011; Inandia et al., 2002; Mohamed et al., 2011).
The literature gives inconsistent findings regarding age as a risk factor. Bener and colleagues (2012) and Kheirabadi and colleagues (2009) found mothers at younger ages were at greater risk for PPD, whereas Green and colleagues (2006) and Rizk and colleagues (2005) found that older age is associated with PPD. In a case-control study conducted by Balaha and colleagues (2009), no differences were obtained. Similar findings were obtained regarding education level. Two studies found higher education as a risk factor for PPD whereas three studies found lower education as a risk factor.
Unemployment was frequently linked to PPD (Bener et al., 2012; Chaaya et al., 2002; Eilat-Tsanani et al., 2006; Inandia et al., 2002; Kheirabadi et al., 2009; Najafi et al., 2007). Although being unemployed may interfere with childcare responsibilities and put additional pressure on women, employed women were at lower risk. Kheirabadi and colleagues (2009) argued that unemployment may be related to poverty that leads to depression. Al-Hinai (2014) found work-related difficulties as a contributing factor in PPD.
Cultural Factors
In studies conducted in the UAE, Jordan, Qatar, and among Middle Eastern/Arab women living in Australia, a poor relationship with the mother in-law was an associated risk factor. Mothers-in-law appear to be important to the success of the marital relationship in these test groups, as sons remain closely tied to their family of origin, often continuing to live with and even work within the family business their entire lives. Mothers-in-law often have a great deal of influence over all aspects of their daughters-in-law and grandchildren’s lives. Therefore a positive relationship with the mother-in-law is important in women’s lives and could lead to depression if it is less than positive (Green et al., 2006). Yount and Smith (2012) argued that the maintenance of ties with (especially female) natal kin will be associated with lower risks of PPD in new mothers. Women’s dependence on patriarchal kin relations, undesired gender of the baby, death of one's father before the age of 13, polygamy, poor relationship with the in-law family, and having a relative with an alcohol problem are also factors unique to these studies. In an interesting study based on focus-group discussions with 19 women (mean age 29 years) and interviews with 9 physicians and 3 health care professionals, the key factors of PPD identified were depression during pregnancy resulting from lack of support from the husband and his family, disagreement between the wife and husband’s family, postnatal depression resulting from difficult delivery, unhealthy or difficult babies, poor bonding with the baby, lack of support and conflict with regard to the mother’s role, and a lack of mother’s understanding of postnatal depression as a type of psychological disorder (Ghubash & Eapen, 2009). These are interrelated sets of factors that could be found in studies of women from other parts of the world. According to some studies, there are not many differences between risk factors observed in the Middle-Eastern/Arab countries and those reported in other places (Alici-Evcimen & Sudak, 2003; Pearlstein, Howard, Salisbury, & Zlotnick, 2009), but the prevalence in the Middle East is certainly higher.
Discussion
The literature review reveals that the prevalence rate of PPD in the target population ranged variably from 10% to 51.8%. Such variation in numbers may be the actual prevalence or it could be a result of methodological limitations of the studies. For example, 51.8% prevalence in Egypt is very high followed by 43% in West Bank and 41% in Iran. These numbers could be even more staggering if the EPDS had included somatization as an indicator of depression because depression in the Middle Eastern/Arab cultures is expressed in more somatic ways. The EPDS is also criticized for focusing on major depressive symptoms, such as “thoughts of self-harm” that may not be very relevant for women from Muslim cultures, as in Islam self-harm or suicidal ideation is considered non-permissible (Yount & Smith, 2012). Additionally, many women may not report any symptoms of PPD as a result of the collectivistic nature of the Middle Eastern society where personal problems are overlooked in the interest of the larger family. When using EPDS, Fritz and McGregor (2013) argue that terms like “mental health” or “depression screen” can be culturally offensive so more neutral communication like “we’d like to know how you are feeling” is more appropriate and the administration of tests should take place preferably in the absence of a family member so the patient can speak more openly. For patients scoring 10 or more on EPDS, further professional referrals may be indicated.
Our review suggests five major domains of risk factors, but the majority of studies focused on psychological and demographic domains and ignored the physical/biological and cultural factors in PPD. Quantitative studies are needed to explore the areas of nutritional deficiencies/metabolic imbalance, hormonal changes, neurotransmitter levels, hypothalamic–pituitary–adrenocortical mechanisms, and iron-deficiency anemia in the development of PPD. The inconsistencies of risk factors may also imply a complex interaction of multiple factors giving rise to PPD and suggest the presence of mediating factors that need further investigation through qualitative research. Validation of EPDS is necessary to obtain more accurate scores and qualitative studies would capture the essence of cultural factors not included in standard assessment tools.
Some Middle Eastern women practice a variety of postpartum rituals including the period of 40 days resting, restricted activities, and diets. During this 40-day period, someone comes to the house or stays with the new mother to take care of the baby, the house, and the other children (Kim-Godwin, 2003). They also receive support from family members including mother, mother-in law, traditional birth attendants, or female relatives (Kim-Godwin, 2003; Klainin & Arthur, 2009). Klaining and Arthur (2009) explained that, “such cultural practices may be perceived as a double-edged sword which offers physical comfort on the one hand but serves as major sources of interpersonal conflicts and emotional frustration on the other.” After delivery, the father or a close male relative calls the Athan (Muslim call to prayer) into the ear of the baby. This is a religious tradition followed by Muslims all over the world.
In some Middle Eastern traditions, women during their postpartum period are fed chicken for protein intake and fenugreek tea with molasses to help with lactation and help replace iron resulting from blood loss during birth. Wrapping cloth around the waist is common and believed to shrink the stomach faster. Cold foods are avoided as it may prolong labor or delivery and hot drinks and soup considered healthy for the baby. Shaving the hair of the baby and giving silver to charity equal to the hair’s weight is also a tradition. The understanding of traditional postpartum practices would help to implement culturally competent perinatal services.
Jarrah and Bond (2007) indicate that although women in the Middle East generally have access to modern health care, many continue to rely on family members for PPD education and this may cause confusion and interpersonal conflicts. Most families in Arab cultures still preserve their traditions and pregnancy and childbirth are celebrated. In many Arabic cultures, the woman’s status may be elevated after becoming a mother and especially after birthing a male child. Denial by many women of PPD as a psychological illness and attributing it to supernatural forces like Jinn or the evil eye is possible and also the ongoing wars in the Middle East may be a contributing factor in psychological health of women including PPD. Research on PPD in the target population is meager to begin with and even smaller on cultural, economic, and political issues affecting PPD.
Implications for prevention and treatment
Research findings suggest that PPD is a serious mood disorder that is historically neglected in the Middle East and leaves mothers to suffer in fear, confusion, and silence (Mohamed et al. 2011). While reasons for neglect of PPD is not researched, one could only surmise that such practices could be a result of lack of scientific knowledge or misunderstandings and the society being so collectivistic that people simply rely on extended family members even for matters including health issues. Research indicates that a single episode of PPD appears to increase the risk of recurrence by 25% for a future delivery (Alici-Evcimen & Sudak, 2003) and mothers who develop PPD are 25% to 100% more likely to experience a recurrent depressive episode in later pregnancies (Gabbe et al., 2007). Therefore, preventative strategies designed to attenuate or eliminate the impact of contributory factors can improve the emotional wellbeing of women in the vulnerable postnatal period (Alici-Evcimen & Sudak, 2003; Bener et al., 2012). The first stage of prevention should start with screening all mothers and especially those who present with potential risk for PPD. The common screening tools for detecting depression are self-report measures of depression, the BDI, BDI-2, Hamilton Rating Scale for Depression, the PDSS, PDPI-R, EPDS, and the EPDS-P. The latter is intended to assess partners of women during the postpartum period. Antenatal screening programs to identify women at risk for psychiatric disorders, including PPD, are recommended by Bener and colleagues (2012) and Mohamed and colleagues (2011). Women should be followed up with during the postnatal period, especially if they have a history of depression or depressive symptoms during pregnancy. A major study of 40,000 perinatal women in Australia strongly recommends screening procedures for depression, but most importantly, culturally relevant diagnostic practices for members of ethnic minorities are recommended (Buist et al., 2007).
After effective screening, preventative factors indicated in the literature are education and increased awareness among women and health care providers with regards to signs and symptoms of PPD (Alici-Evcimen & Sudak, 2003; Bener et al., 2012). While this approach is common in the West, it is severely lacking in Middle Eastern countries, perhaps due to the notion that they already know what to do and perhaps due to their refusal to compromise their traditional practices.
Treatment of PPD should also be multifactorial, including consideration of psychosocial as well as pharmacological options. Adequate recognition and treatment of postpartum depression is essential to the health and wellbeing of the mother, the infant, and the family (Suri & Altshuler, 2004). Psychosocial therapies and pharmacotherapy are the two main treatment options available, but their use in this part of the world is quite limited (Alici-Evcimen & Sudak, 2003; Pearlstein, Howard, Salisbury, & Zlotnick, 2009). Studies recommend that new mothers should be encouraged to express their feelings and let go of their guilt that may be associated with the symptomology of PPD (Bener et al., 2012; Mohamed et al., 2011). In addition, research also supports the idea of developing support groups during antenatal and prenatal periods, enhancing individual’s self-esteem, and focusing on improving partner relationships (Mohamed et al., 2011). Interpersonal Psychotherapy (ITP), which is a short-term treatment for Manic Depressive Disorder and addresses interpersonal issues, such as role change, marital relationship, social support, and life stressors may be highly effective for some women and could be especially well-suited for Arab cultures due to the collectivistic nature of their society (Pearlstein, Howard, Salisbury, & Zlotnick, 2009; O’Hara, 1995).
Other effective treatments indicated in the literature are group psychotherapy (Clark et al., 2003; Goodman & Santangelo, 2011), hormone therapy (Williamson & McCutcheon, 2004), and mother-infant psychotherapy that emphasize the significance of fear and loss in the disturbed mother-infant interactions (Clark et al., 2003; Guedeney et al., 2011). A majority of empirical studies conducted in primary prevention also suggest that psychotherapy should be considered as a first-line treatment rather than an adjunct to medication (Stuart, O’Hara, & Gorman, 2003). In addition, there is growing recognition and acceptance of exercise as a useful treatment option for depression, especially among postpartum women who are reluctant to take medication and when psychological therapies are not available (Daley, MacArthur, & Winter, 2007).
Based on existing research however, no definite conclusions could be drawn about long-term effects of psychological treatments when compared to pharmacological interventions (Cuijpers, Brannmark, & van Straten, 2008). Since breastfeeding is practiced commonly among Middle-Eastern women, pharmacotherapy should be carefully evaluated as it poses a risk of transmitting medication to the infant through breast milk, which could result in harmful exposures. Risk-benefit assessment of prescription medication should be made in consultation with medical and mental health experts. Medication should only be prescribed when symptoms of depression are severe and there is high risk for self-harm or harm to the baby (Alici-Evcimen & Sudak, 2003). However, the American Congress for Obstetrics and Gynecology (ACOG, 2009) recommends use of Selective Serotonin Reuptake Inhibitors (SSRI anti-depressants such as Sertraline) because they are relatively safe. It is important that the obstetricians and mental health team work in collaboration for maximum patient benefit.
Research also indicates that incorporating culture-bound practices and rituals into mainstream therapeutic procedures and training of health care workers in the detection and management of postnatal depression can have beneficial effects (Ghubash & Eapen, 2009; Kim-Godwin, 2003). In a study by Nahas and Amasheh (1999), Jordanian women defined postpartum care in terms of strong family support and kinship, and preservation of childbearing customs as expressed in the celebration of the birth of the baby. These rituals were found to be of supportive value and helped to facilitate transition to motherhood (Dennis et al., 2007; Grigoriadis et al., 2009).
Given the high prevalence of religious beliefs among Middle-Eastern/Arab populations, religious coping strategies may have an important preventive and therapeutic effect. Doucet and Letourneau (2009) outline that religious faith and coping can contribute to a decrease in low self-esteem and suicidal ideations that may be present in women diagnosed with PPD. Koenig (2009) found that religious beliefs and practices could represent powerful sources of comfort, hope, and meaning. In a similar vein, a study by Zittel-Palamara, Cercone, and Rockmaker (2009) indicated that nearly 66% of the postpartum women found strength in religion. Religious rituals and practices are quite common in the Arab world but empirical studies in the context of PPD are nonexistent. Traditional healing practices for psychological disorders may prove helpful for this population (Haque & Keshavarzi, 2014; Ghubash & Eapen, 2009).
The limited number of existing studies in this review was highly selective and used convenience samples, making generalizability and comparability of results difficult. A majority of the studies employed hospital-based samples, excluding the population of women who delivered in local or private settings, resulting in a less diverse sample. Further, studies varied significantly regarding cut off scores on the EPDS and the time frame employed, ranging from 2 days to 13 months with only a few studies using the time frame specified by the DSM-V (4 weeks) diagnostic criteria. In many studies, assessment of risk factors of PPD was not made using standardized and validated instruments, resulting in questionable validity of the results. In addition, only a few studies assessed depression during both pregnancy and postpartum period. Finally, absence of a control group was a major limitation of these studies. Since all studies conducted in Middle-Eastern/Arab countries were included regardless of their reliability and internal validity, the research findings may be questionable.
This study provides evidence that a considerable proportion of Middle-Eastern/Arab women experience deterioration in their psychological health and social adjustment after delivery as well as during pregnancy. The literature review demonstrates a need for future research with a focus on the development of proper screening tools and consideration of cultural factors in the treatment of this group. It is also important that further psychologically valid research studies occur in order to gain a more in-depth understanding of how PPD affects this population. Health care providers need to be aware of and receive appropriate training on psychological issues when providing care for women who are pregnant and who have recently given birth. Women should also be prepared for possible adjustment problems after the birth and should be taught coping strategies to prevent PPD.
References
- Abou-Saleh, M. T., & Ghubash, R. (1997). The prevalence of early psychiatric morbidity in Dubai: A transcultural perspective. Acta Psychiatrica Scandinavica, 95, 428-432.
- Affonso, D. D., De, A. K., Horowitz, J. A., & Mayberry, L. J. (2000). An international study exploring levels of postpartum depressive symptomatology. Journal of Psychosomatic Research, 49, 207–216.
- Agoub, M., Moussaoui, D., & Battas, O. (2005). Prevalence of postpartum depression in a Moroccan sample. Archives of Women’s Mental Health, 8, 37-43. DOI 10.1007/s00737-005-0069-9.
- Al-Hinai, F. I. (2014). Prospective study on prevalence and risk factors of postpartum depression in Al Dakhliya Governorate in Oman. Oman Medical Journal, 29, 198-202.
- Alici-Evcimen, Y., & Sudak, D. M. (2003). Postpartum depression. Psychiatry Updates, 10, 210-216.
- Alkar, Ö., & Gençöz, T. (2005). Critical factors associated with early postpartum depression among Turkish women. Contemporary Family Therapy, 27, 263-275. doi: 10.1007/s10591-005-4043-5
- American Congress of Obstetrics and Gynecology (2009). Depression during pregnancy: Treatment recommendations. Retrieved from http://www.acog.org/About-ACOG/News-Room/News-Releases/2009/Depression-During-Pregnancy
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: APA.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: APA.
- Amr, M.A.M. & Balaha, M.H.H. (2010). Minor psychiatric morbidity in young Saudi mothers using Mini International Neuropsychiatric Interview (MINI) [Abstract]. Journal of the College of Physicians and Surgeons Pakistan, 20, 680-684.
- Balaha, M. H., Amr, M. A., El-Gilany, A. A., & Al Sheikh, F. M. (2009). Obstetric and Psychiatric Outcomes in a Sample of Saudi Teen-Aged Mothers. TAF Preventive Medicine Bulletin, 8, 285-290.
- Bashiri, N & Spielvogel, A. M (1999). Postpartum Depression: A Cross-cultural Perspective. Psychiatry Update, 6(3), 82-87.
- Beck, C.T. (1993). Teetering on the edge: A substantive theory of postpartum depression. Nursing Research, 42-48.
- Bener, A., Gerber, L. M., & Sheikh, J. (2012). Prevalence of psychiatric disorders and associated risk factors in women during their postpartum period: A major public health problem and global comparison. International Journal of Women’s Health, 4, 191-200.
- Bowen, A., Bowen, R., Butt, P., Rahman, K., & Muhajarine, N. (2012). Patterns of Depression and Treatment in Pregnant and Postpartum Women. Canadian Journal of Psychiatry, 57, 161-167.
- Bugdayci, C. R., Sasmaz, T., Tezcan, H., Kurt, A. O., & Öner, S. (2004). A cross-sectional prevalence study of depression at various times after delivery in Mersin province in Turkey. Journal of Women's Health, 13, 63-68.
- Buist, A., Ellwood, D., Brooks, J., Milgrom, J., Hayes, B.A., Sved-Williams, A., et al. (2007). National program for depression associated with childbirth: the Australian experience. Clinical Obstetrics and Gynecology, 21, 193-206.
- Chaaya, M., Campbell, O. M. R., El Kak, F., Shaar, D., Harb, H., & Kaddour, A. (2002). Postpartum depression: Prevalence and determinants in Lebanon. Archives of Women’s Mental Health, 5, 65-72.
- Clark, R., Wenzel, A., & Tluczek, A. (2003). Psychotherapy for postpartum depression: A preliminary report. American Journal of Orthopsychiatry, 73, 441-454.
- Cuijpers, P., Brannmark, J. G., & van Straten, A. (2008). Psychological treatment of postpartum depression: A meta-analysis. Journal of Clinical Psychology, 64, 103-118.
- Daley, A. J., MacArthur, C., & Winter, H. (2007). The role of exercise in treating postpartum depression: A review of the literature. Journal of Midwifery & Women’s Health, 52, 56-62.
- Danaci, A. E., Dinç, G., Deveci,A. Sen, F.S. & Içelli. I. (2002). Postnatal depression in Turkey: Epidemiological and cultural aspects. Social Psychiatry and Psychiatric Epidemiology, 37, 125-129.
- Dennis, C. L., Fung, K., Grigoriadis, S., Robinson, G. E., Romans, S., & Ross, L. (2007). Traditional postpartum practices and rituals: A qualitative systematic review. Women's Health, 3, 487-502.
- Doucette, S. S., & Letourneau, N. N. (2009). Coping and suicidal ideations in women with symptoms of postpartum depression. Clinical Medicine: Reproductive Health, 2, 9-19.
- Eilat-Tsanani, S., Merom, A., Romano, S., Reshef, A., Lavi, I., & Tabenkin, H. (2006). The effect of postpartum depression on women’s consultations with physicians. Israel Medical Association Journal, 8, 406-410.
- Evins, G.G., Theofrastous, J. P. & Galvin, S.L. (2000). Postpartum depression: A comparison of screening and routine clinical evaluation. American Journal of Obstetrics and Gynecology, 182, 1080-1082.
- Fritz, B., & McGregor, C. (2013). Postpartum depression screening in Yemeni and Punjabi immigrant women. Nursing for Women’s Health, 17, 236-244.
- Fuggle P., Glover, L., Khan, F., & Haydon, K. (2002). Screening for postnatal depression in Bengali women. Journal of Reproductive and Infant Psychology 20(2), 71-82.
- Gabbe, S. G., Niebyl, J. R., Landon, M., Simpson, J. L., & , Goetzl, J. (2007). Obstetrics: Normal and problem pregnancies (5th ed). Philadelphia, PA: Elsevier.
- Ghubash, R., & Eapen, V. (2009). Postpartum mental illness: Perspectives from an Arabian Gulf population. Psychological Report, 105, 127-36.
- Glasser, S., Stoski, E. & Kneler, V. (2011). Postpartum depression among Israeli Bedouin women, Archives of Women’s Health, 14, 203-208.
- Glavin, K., Smith, L., & Sørum, R. (2009). Prevalence of postpartum depression in two municipalities in Norway. Scandinavian Journal of Caring Sciences, 23, 705-710.
- Grace, S.L., Evindar, A., & Stewart, D.E. (2003). The effect of postpartum depression on child cognitive development and behavior: A review and critical analysis of literature. Archives of Women’s Mental Health, 6, 263-274.
- Goodman, J.H. & Sanatangelo, G. (2011). Group treatment for postpartum depression: A systematic review. Archives of Women’s Mental Health, 14, 277-293.
- Green, K., Broome, H., & Mirabella, J. (2006). Postnatal depression among mothers in the United Arab Emirates: Socio-cultural and physical factors. Psychology, Health & Medicine, 11, 425-431.
- Grigoriadis, S., Robinson, G. E., Fung, K., Ross, L. E, Chee, C., Dennis, C. E. et al. (2009). Traditional postpartum practices and rituals: Clinical implications. Canadian Journal of Psychiatry, 54, 834-840.
- Guedeney, A., Guedeney, N., Tereno, S., Dugravier, R., Greacen, T., Welniarz, B. et al. (2011). The time of the infant, parent-infant desynchronization and attachment disorganization. Retrieved from http://uqam.academia.edu
- Hamdan, A., & Tamim, H. (2011). Psychosocial risk and protective factors for postpartum depression in the United Arab Emirates. Archives of Women's Mental Health, 14(2), 125–133.
- Haque, A. (2010). Mental health concepts in Southeast Asia: Diagnostic considerations and treatment implications. Psychology, Health & Medicine, 15 (2), 127-134.
- Haque, A. & Keshavarzi, H. (2014). Integrating indigenous healing methods in therapy: Muslim beliefs and practices. International Journal of Culture and Mental Health, 7, 297-314.
- Inandi, T., Elci, O. C., Ozturk, A., Egri, M., Polat, A., & Sahin, T. K. (2002). Risk factors for depression in postnatal first year, in eastern Turkey. International Journal of Epidemiology, 31, 1201-1207.
- Jarrah, S. & Bond, A.E. (2007). Jordanian women's postpartum beliefs: An exploratory study. International Journal of Nursing Practice, 13, 289-193.
- Khalaf, I. A., Abu-Moghli, F. A., Mahadeen, A. I, Callister, L. C., & Al-Hadidi, M. (2007). Jordanian women’s perceptions of post-partum health care. International Nursing Review, 54, 288–294.
- Kheirabadi, G.R., Maracy, M. R., Barekatain, M., Salehi, M., Sadri, G.H., Kelishadi, M. (2009). Risk factors of postpartum depression in rural areas of Isfahan Province, Iran. Archives of Iranian Medicine, 12, 461-467.
- Kim-Godwin, Y. S. (2003). Postpartum beliefs and practices among non-western cultures. The American Journal of Maternal/Child Nursing, 28(2), 74-78.
- Klainin, P., & Arthur, D. G. (2009).Postpartum depression in Asian cultures: A literature review. International Journal of Nursing Studies, 46, 1355-1373.
- Koenig, H. G. (2009). Research on religion, spirituality, and mental health: A review. The Canadian Journal of Psychiatry, 54, 283-291.
- Lanes, A., Kuk, J. L., & Tamim, H. (2011). Prevalence and characteristics of postpartum depression symptomatology among Canadian women: A cross-sectional study. BMC Public Health, 11, 302. doi:10.1186/1471-2458-11-302.
- Lee King, P. (2012). Replicability of structural models of the Edinburgh Postnatal Depression Scale (EPDS) in a community sample of postpartum African American women with low socioeconomic status. Archives Of Women's Mental Health, 15(2), 77-86. doi:10.1007/s00737-012-0260-8.
- Masmoudi, J., Tabelsi, S., Charfeddine, F., Ben Ayed, B., Guermazzi, M., & Jaoua, A. (2008). Study of the prevalence of postpartum depression among 213 Tunisian parturients. Gyne´cologie Obste´trique & Fertilite´, 36, 782-787.
- Mathers‚ C. D. & Loncar, D. (2006). Projections of global mortality and burden of disease from 2002 to 2030. Pathogens Neglected Tropical Diseases (PLOS) Medicine‚ 3(11)‚ doi: http://dx.doi.org/10.1371/journal.pmed.0030442
- Misri, S. H. (2005). Pregnancy blues: What every woman needs to know about depression during pregnancy. Westminster, MD: Dell Publishing.
- Mohamed, N. A., Mahmoud, G. A., Said, N. A., Abdelhafez, H. A., & Maklof, A. M. A. (2011). Postpartum depression: Prevalence and predictors among women at El Eman's Specialized Hospital. Journal of American Science, 7(12), 122-128.
- Mohammad, K. I., Gamble, J., & Creedy, D. K. (2011). Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. Midwifery and Women’s Health, 27, e238–e245.
- Nahas, V., & Amasheh, N. (1999). Culture care meanings and experiences of postpartum depression among Jordanian Australian women: A transcultural study. Journal of Transcultural Nursing, 10, 37-45.
- Nahas, V. L., Hillege, S., & Amasheh, N. (1999). Postpartum depression: The lived experiences of Middle Eastern migrant women in Australia. Journal of Nurse-Midwifery, 44, 65-74.
- Najafi, K., Zarrabi, H., Shirazi, M., Avakh, F., & Nazifi, F. (2007). Prevalence of postpartum depression in a group of women delivering at a hospital in Rasht city, Iran. Journal of Pakistan Psychiatric Society, 4(2).
- Nonacs, R. & Cohen, L.S. (2000). Postpartum psychiatric syndromes. In B. Sadock & V. Sadock. (Eds.), Comprehensive Textbook of Psychiatry (7th ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
- O’Mahoney, J. & Donelley, T. (2010). Immigrant and refugee women’s postpartum depression help and access to care: A review and analysis of the literature. Journal of Psychiatric and Mental Health Nursing, 17, 917-928.
- O’Hara, M. W. (1995). Interpersonal Psychotherapy for Postpartum Depression. Women's Health Issues, 5(2), 75-76.
- Pearlstein, T., Howard, M., Salisbury, A., & Zlotnick, C. (2009). Postpartum depression. American Journal of Obstetrics and Gynecology, 200, 357-364.
- Reck, C., Struben, K., Backenstrass, M., Stefenelli, U., Reinig, K., Fuchs, T. et al. (2008). Prevalence, onset and comorbidity of postpartum anxiety and depressive disorders. Acta Psychiatrica Scandinavica, 118, 459-468. doi:10.1111/j.1600-0447.2008.01264.x
- Rizk, D. E., Nasser, M., Thomas, L. & Ezimokhai, M. (2005). Women’s perceptions and experiences of childbirth in United Arab Emirates. Journal of Perinatal Medicine, 29, 298-307.
- Rouhi, M., Usefi, H., & Alizade, S. M. (2009). Postpartum health care seeking in Iran. International Journal of Gynecology & Obstetrics, 107. doi:10.1016/S0020-7292(09)61809-9
- Roysircar, G. (2005). Research in multicultural counseling: Client needs and counselor competencies. In C. Lee (Ed.), Multicultural issues in counseling: New approaches to diversity (3rd ed.). Alexandria, VA: American Counseling Association.
- Azar, A. S., Hashemi, Z., & Forghani, F. (2006). Postpartum depression and its correlates among women living in Zabol (Iran). Iranian Journal of Psychiatry, 1, 140-147.
- Segre, L. S. & Davis, N. D. (2013). Postpartum depression and perinatal mood disorders in the DSM. Retrieved from: Postpartum International. www.postpartum.net
- Segre, L. S., O’Hara, M. W., Arndt, S., & Stuart, S. (2007). The prevalence of postpartum depression: The relative significance of three social status indices. Social Psychiatry & Psychiatric Epidemiology, 42, 316-321.
- Sharifi, K. H., Sooky, Z. Tagharrobi, Z., & Akbari, H. (2007). The assessment of postpartum depression and ‘‘satisfaction from husband’’. European Psychiatry, 22(1), S66-S67.
- Sharifi, K. H., Sooky, Z. Tagharrobi, Z., & Akbari, H. (2007). Relationship between kind of delivery and postpartum depression. European Psychiatry, 22(1), S245–S246.
- Stewart, D. E., Robertson, E., Dennis, C. L., Grace, S. L., & Wallington, T. (2003). Postpartum depression: Literature review of risk factors and interventions. Retrieved from http://www.who.int/mental_health/prevention/suicide/lit_review_postpartum_depression.pdf.
- Stone, K. (2013). What the new DSM-V says about postpartum depression & psychosis. Retrieved from http://www.postpartumprogress.com/what-the-new-dsm-v-says-about-postpartum-depression-psychosis
- Stuart, S. (2012). Interpersonal psychotherapy for postpartum depression. Clinical Psychology and Psychotherapy, 19, 134-140.
- Stuart, S., O’Hara, M.W., & Gorman, L. K. (2003). The prevention and psychotherapeutic treatment of postpartum depression. Archives of Women’s Mental Health, 6, S57-S69.
- Suri, R., & Altshuler, L.L. (2004). Postpartum depression: Risk factors and treatment options. Psychiatric Times, 21(11), p.64.
- Tammentie, T., Tarka, M. T., Astedt-Kurki, P., & Paavilainen, E. (2002). Sociodemographic factors of families related to postnatal depressive symptoms of mothers. International Journal of Nursing Practice, 8, 240-246.
- Yount, K. M., & Smith, S. M. (2012). Gender and postpartum depression in Arab Middle Eastern women. Women's Studies International Forum, doi:10.1016/j.wsif.2012.03.017.
- Williamson, V., & McCutcheon, H. (2004). Postnatal depression: A review of current literature. Australian Midwifery: Journal of the Australian College of Midwives, 17(4), 11-16.
- Wisner, K., Chambers, C. & Sit, D. (2006). Postpartum depression: A major public health problem. Journal of American Medical Association, 229, 2616-2618.
- World Health Organization (WHO). (2003). Managing complications in pregnancy and childbirth: A guide for midwives and doctors. The Department of Reproductive Health and Research, WHO. Retrieved from http://www.who.int/reproductive-health/impac/Clinical_Principles/Emotional_support_C7_C14html.
- Zangene, M., Alizadeh, N. S., Rezaei, F., Rezaei, M. (2011). Depression prevalence and its relationship with delivery method in Iranian women. European Psychiatry, 26(1), 1870.
- Zittel-Palamara, K., Cercone, S. A., & Rockmaker, J. R. (2009). Spiritual support for women with postpartum depression. Journal of Psychology and Christianity, 28(3), 213-223.